Hospitals may be discharging XDR-TB patients too soon – study


Published online today in the medical journal, The Lancet, the research followed 107 XDR-TB patients from three hospitals Cape Town, Uppington and Johannesburg for five years. During the course of the study, about 40 percent of the patients were eventually discharged.
However, researchers found that of those who had been discharged, about 40 percent were not cured at the time they were sent home and a about third of these patients were at a high risk of transmitting the disease, according to the study conducted by the University of Cape Town (UCT), Stellenbosch University and the US Emory University School of Medicine.
The study is the first to suggest that South African hospitals may be discharging more XDR-TB patients before they are fully cured than previously thought, according to one of the researchers, Keertan Dheda, a professor at UCT’s department of medicine.
“Alarmingly, we have shown for the first time that… treatment failure, and discharge of such patients into the wider community, is occurring systematically on a country-wide level in South Africa,” said Dheda, who added that many hospitals feel pressure to discharge patients due to the scarce number of beds available. “We think (these findings) are a mirror of what is happening on a wider scale.”
Dheda and his team also recorded at least one instance in which a patient had transmitted the diseases to a relative. The patient and his brother both eventually died, as did almost two-thirds of all patients enrolled in the study.
XDR-TB is resistant to both of the most commonly used anti-TB drugs, isoniazid and rifampin, as well as at least one second-line drug. With a limited number of drugs available to treat the disease, patients who do not respond to treatment often run out of other options.
However, some doctors have caution that discharged XDR-TB patients are not the source of South Africa’s large XDR-TB problem.
Dr Gilles van Cutsem is the South African medical coordinator for international humanitarian organisation Medicines Sans Frontières (MSF). He says that people are much more likely to contract XDR-TB from people who have not been diagnosed and started treatment than they are from those who have been discharged from hospitals.
“Yes, some people are getting infected by people who have been discharged or are failing treatment but the majority of transmission doesn’t happen like that,” van Cutsem told Health-e. “The majority of transmission is by people who haven’t been diagnosed and started on treatment.”
Decentralisation a move in the right direction

What is clear from Dheda’s research is that government’s 2012 decision to decentralise the treatment of multidrug-resistant TB (MDR-TB) has been a step in the right direction. While resistant to fewer treatments than XDR-TB, MDR-TB is also resistant to isoniazid and rifampin.
“MDR-TB has been officially decentralised…that makes treatment much more accessible,” Dheda added. “The official policy is still to admit XDR-TB patients into facilities but with the sheer burden of disease it wont be long before that is also decentralised.”
In his Lancet article, Dheda and his co-authors advocate for the expansion of community-based, in-patient XDR-TB treatment centres that are linked with good home-based and palliative care services as an answer to South Africa’s shortage of beds. This approach has already been pioneered in the Western Cape by MSF, which recently handed its XDR-TB treatment centre – Lizo Nobanda – over to St Luke’s Hospice.
Located in Khayelitsha, Lizo Nobanda allowed XDR-TB patients to stay for months at the centre to complete or re-start treatment and get help dealing with the sometimes-crippling side effects of treatment.
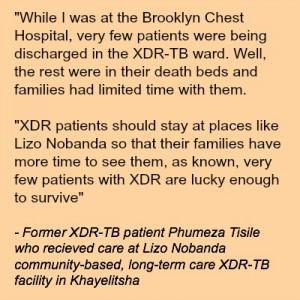
Phumeza Tisile is one of the lucky ones. The former Lizo Nobanda patient was officially cured of XDR-TB in August after years of treatment. She calls being cured “a miracle.”
“Imagine this – just a few months back you are told that you must prepare your soul for death because there is no way that you can survive and that the doctors have run out of options,” says Tisile of being cured. “Then a few weeks later they are singing a different tune… it is so exciting to be told you are no loner dying”
Tisile also spent time in Cape Town’s Brooklyn Chest Hospital and says that the move to Lizo Nobanda allowed her to be closer to her family – and made treatment feel like less of a prison.
“At Lizo Nobanda there were no visiting hours so visitors can stay as long as they wish, and the patients are free – we weren’t locked up in rooms like in the big hospitals,” she remembers.
“Even the nurses were not the same,” she adds.
While community-based care may not be cheaper than hospital admissions, the advantages to patients may be priceless, according to van Cutsem who says he thinks South Africa will see more treatment facilities like it in the future to help control the country’s XDR-TB epidemic.
While Lizo Nobanda was a standalone facility, other community-based approaches could include XDR-TB wards at district hospitals or an nonprofit-run hospice approach.
“We started Lizo Nobanda as part of the decentralisation programme because we wanted to look at treating patients as much as possible in their communities,” he said. “We need to establish more Lizo Nobanda-type facilities that provide community-based, in-patient facilities where patients can…be admitted for a longer time but in a more humane environment.” – Health-e News Service.
Author
Republish this article
This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
Unless otherwise noted, you can republish our articles for free under a Creative Commons license. Here’s what you need to know:
You have to credit Health-e News. In the byline, we prefer “Author Name, Publication.” At the top of the text of your story, include a line that reads: “This story was originally published by Health-e News.” You must link the word “Health-e News” to the original URL of the story.
You must include all of the links from our story, including our newsletter sign up link.
If you use canonical metadata, please use the Health-e News URL. For more information about canonical metadata, click here.
You can’t edit our material, except to reflect relative changes in time, location and editorial style. (For example, “yesterday” can be changed to “last week”)
You have no rights to sell, license, syndicate, or otherwise represent yourself as the authorized owner of our material to any third parties. This means that you cannot actively publish or submit our work for syndication to third party platforms or apps like Apple News or Google News. Health-e News understands that publishers cannot fully control when certain third parties automatically summarise or crawl content from publishers’ own sites.
You can’t republish our material wholesale, or automatically; you need to select stories to be republished individually.
If you share republished stories on social media, we’d appreciate being tagged in your posts. You can find us on Twitter @HealthENews, Instagram @healthenews, and Facebook Health-e News Service.
You can grab HTML code for our stories easily. Click on the Creative Commons logo on our stories. You’ll find it with the other share buttons.
If you have any other questions, contact info@health-e.org.za.
Hospitals may be discharging XDR-TB patients too soon – study
by lauralopez, Health-e News
January 17, 2014



